Predicting response to immune checkpoint blockades in high-grade soft tissue sarcomas

Project summary
Objectives: Sarcomas are rare cancers found in bones and soft tissues, such as muscles. Unfortunately, most sarcoma patients do not respond well to current treatment approaches, and often the tumour spreads to different parts of the body and becomes fatal. In this project, we will develop new computational approaches that can help predict which patients could respond to new treatment strategies that engage the patient’s own immune system in the fight against tumour cells. Our goals are to learn which biological variables influence the therapeutic response and to support clinical decision-making to accelerate access to immune therapies.
Previous Research: Tumour-fighting immune cells (T-cells) recognize mutations in cancer cells, but their overall success depends on a number of important factors. These include the extent to which mutations change the tumour’s proteins, whether they are in a few or many tumour cells, and whether they are obvious to or hidden from the immune system. Furthermore, T-cells can be turned off by specific signals in the tumour ecosystem, or blocked from entering in the first place. New immune-based therapies counteract the signals that stop T-cells from working well, enabling them to re-engage in the fight against cancer, and some sarcoma patients have shown good responses to these therapies in recent clinical trials, Whether this blockade is successful can be measured by studying the DNA, RNA, and proteins in a tumour. We have established computational approaches to identify how the immune-relevant factors mentioned above change between patients, and whether some combinations are associated with better therapeutic responses.
Project Methods: We have generated a large collection of molecular data from sarcoma patients with different types, allowing us to deeply analyze the immune cell composition within tumours and the capacity for tumour mutations to instigate an immune response. Using computational and machine learning approaches that leverage all molecular layers (DNA, RNA, protein), we will establish which factors (e.g. immune cell types and diversity, mutations, etc.), or which combinations of factors, are most important in predicting improved response to immune-activating therapies.
Impact and Relevance to Cancer: This work will improve our understanding of sarcoma tumour immunobiology, and accelerate the development of strategies to predict immune-therapy treatment responses in individual patients. In close collaboration with our sarcoma clinical team, we will share immune therapy-relevant findings within a clinical reporting system, to help bridge research and clinical practice.
Quotes
“Many sarcoma patients encounter relapses or metastases despite the standard-of-care. Our research focuses on machine learning-based prediction of therapeutic responses to immune checkpoint blockade, which a subset of sarcoma patients benefit from. With this valuable opportunity supported by the TFRI and MOHCCN, I am grateful to be able to contribute to bringing hope to patients by providing scientific evidence based on the patient data collected within the Canadian community, enabling their access to newer treatments.”
- Hyojin Song, HI&DS Award recipient
“The MOHCCN is generating molecular profiling data from many sarcoma patients, providing a unique opportunity to develop strategies that can help stratify those expected to benefit from immunotherapies. Hyojin’s work, supported by the MOHCCN HI&DS award, will use machine learning approaches to shed light on the molecular characteristics of immunotherapy responders versus non-responders. Her approach integrates both MOHCCN and external datasets for discovery of biomarkers, and powers development of novel stratification approaches suitable for translation.”
- Dr. Sorana Morrissy, mentor
Key Researcher
-
Hyojin
Chercheur
Song
Nouvelles
-
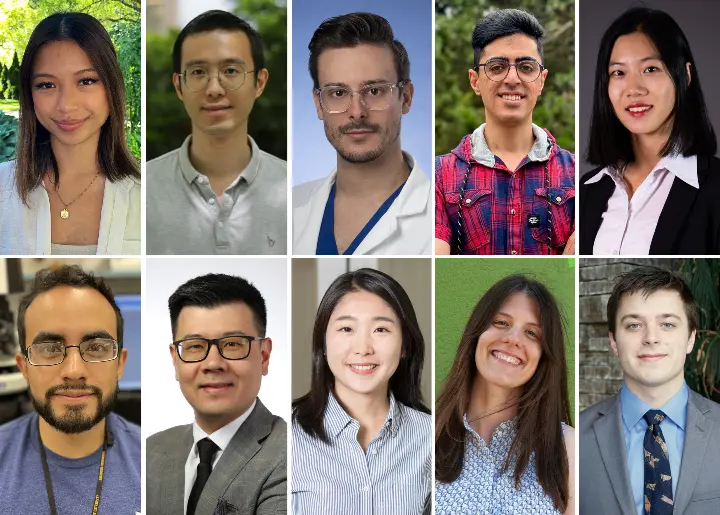
Le Réseau désigne 10 scientifiques des données en début de carrière comme lauréats de sa bourse Marathon de l’espoir pour informatiques de la santé & science des données 2024
Chacun d'entre eux recevra 40 000 dollars du Réseau au cours de l'année prochaine, qui seront complétés par leur établissement d'accueil, pour un total de 80 000 dollars, afin de soutenir la recherche...
